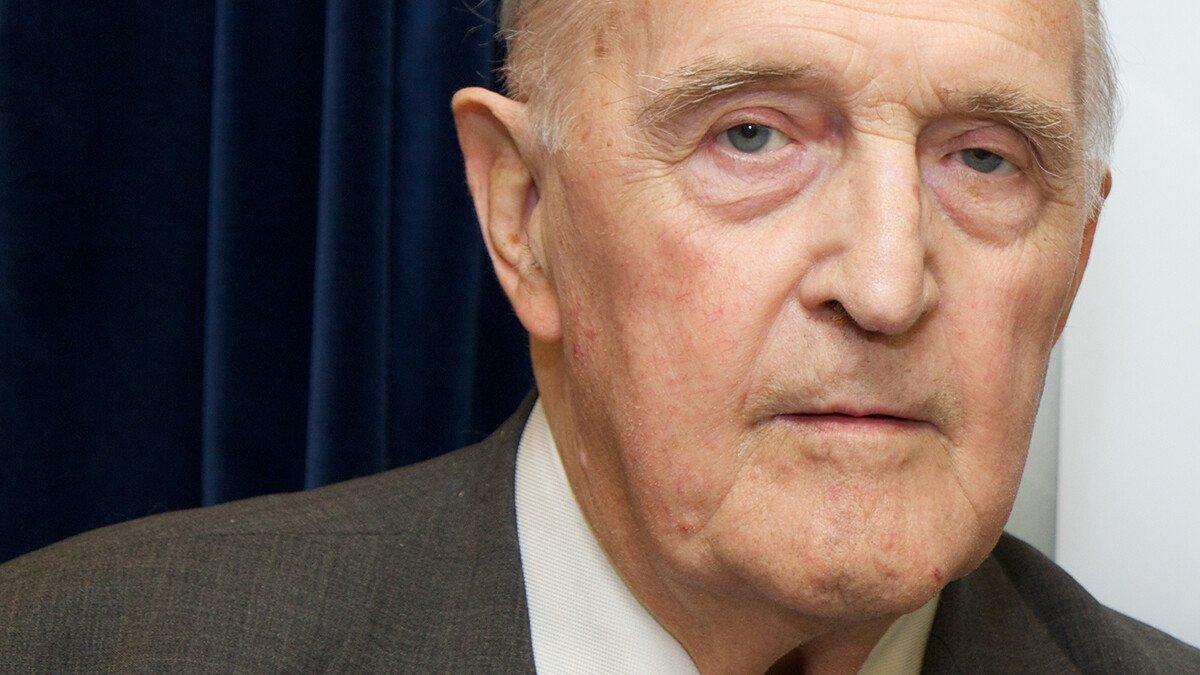
Sir David Weatherall, 1933-2018
A doctor and scientist of great compassion and intellect, Sir David Weatherall died on 8 December 2018. He was a member of Wellcome’s Board throughout the 1990s, helping to shape our support for science, particularly research in tropical medicine and genetics.
In his speech accepting the 2010 Lasker-Koshland Special Achievement Award in Medical Science, Sir David Weatherall credited two "chance events" for the direction of his career.
First, two years after qualifying as a doctor at Liverpool University, being posted to Singapore for National Service in 1958. Put in charge of the Children’s Ward in the British Military Hospital, one of his first patients was a profoundly anaemic young girl being kept alive only with monthly blood transfusions. He discovered that she had thalassaemia, which sparked a lifelong interest in inherited blood disorders and tropical medicine.
His first published research paper was a case report of this child, the daughter of a Nepalese Ghurka soldier serving in the British Army. According to Sir David, he was soon informed by his superiors that he could be court-martialled for publishing material about the Army without permission: "Never do it again," he remembered being told. "And anyway, it is bad form to tell the world that our best regiments have got bad genes." Fortunately, he ignored that piece of careers advice.
The second event was being asked to go on a two-month tour of Asia in 1967 to report on the clinical importance of thalassaemia for the World Health Organization. In the intervening years, he had done ground-breaking research into the clinical and molecular features of the disease. On this trip, he met many people who would become long-term collaborators and partners.
Basic science and clinical applications
Thalassaemia is caused by problems in the body’s production of haemoglobin. In 1965, David Weatherall and John Clegg uncovered how different forms of the disease related to problems in the synthesis of different chains of protein in haemoglobin. In the course of their work, they developed a way to measure the rate of production of these chains in test-tubes, which soon became the basis of a prenatal test for the disease and remained the standard until DNA testing took over in the 1980s.
Being able to apply knowledge gained through basic research to controlling and preventing illness was an important principle for the institute that Sir David established at Oxford University in 1989. Today, it is known as the MRC Weatherall Institute for Molecular Medicine ("the WIMM"), and it was one of the first places where clinicians in training and PhD students in cell and molecular biology could work together, tackling the same problems and learning from each other.
Weatherall and Wellcome
In 1978, the Director of Wellcome, Peter Williams, wanted to increase support for tropical medicine. He met David Weatherall, who was by then the Nuffield Professor of Clinical Medicine at Oxford University, and they worked together with other colleagues to establish a number of partnerships between Wellcome, Oxford and institutions in Thailand (1979), Kenya (1989) and Vietnam (1992).
These partnerships have today developed into three of Wellcome’s Asia and Africa programmes. For many years, they were led by scientists who had studied at the WIMM, notably Nick White in Thailand, Kevin Marsh in Kenya and Jeremy Farrar (the current Director of Wellcome) in Vietnam. Foremost in these programmes was Sir David’s focus on clinical medicine and public health allied to world-leading basic science, and an ethos of equal partnership between the countries, the institutions and the people working in them.
Sir David was a Trustee (later Governor) of Wellcome from 1990 to 2000, working with then-Chairman Sir Roger Gibbs to oversee the transition of Wellcome into an independent foundation. It was also a period of exciting scientific advances, notably the rise of genetics and the Human Genome Project in particular. Sir David, whose work had gone on to detail the genetic changes underlying different types of thalassaemia, remained engaged with issues in scientific and medical training, the ethics of research, and how to communicate findings to the public.
In addition to his many achievements, Sir David will be remembered for his great passion for clinical medicine, his compassion for every patient and their families, his wisdom and intellect, and his impish, self-effacing sense of humour. He was an optimist and a much-appreciated mentor, someone who inspired others to achieve more than they themselves thought possible.
When he had begun applying the tools of molecular biology to help his patients, it was considered unusual; today, it is a fundamental part of clinical medicine and research, thanks in large part to Sir David’s enduring legacy. He was one of the world’s most influential and impactful clinical scientists of the last 50 years.