Covid-19: how researchers around the world are racing to understand the virus and prevent future outbreaks
As Covid-19 continues to spread around the world, a global community of researchers are working to find out more about the virus and assess what research needs to be done to stop it and prevent future outbreaks.
Here’s the latest on some of the key questions that researchers are working to answer.
Where did Covid-19 come from?
We know that Covid-19 is caused by a newly discovered type of coronavirus (SARS-CoV2), but we don’t yet know where the virus originated.
We do know that coronaviruses spread among animals and they are zoonotic – meaning sometimes they can pass from animals to people.
Rapid genetic sequencing of the virus has shown that it is very similar to a known bat virus found in China, and to the SARS coronavirus which spread rapidly in 2002. It’s likely that the virus originated in bats, but current theories suggest an intermediate animal passed it on to humans. Studies are underway to help researchers understand which animal transmitted the virus and how, and what is needed to prevent infections from animals in future.
Rumours and misinformation have circulated on its origin, including a theory that the virus was man-made. However, a Wellcome-supported analysis of the virus genome, led by researchers at Scripps Research, has confirmed that the virus was not made in a laboratory or otherwise engineered.
How does the disease spread and how deadly is it?
Covid-19 is a disease that spreads from person to person. When an infected person coughs or exhales, respiratory droplets are dispersed in the air or on surfaces. These droplets can infect other people directly, or infect those who touch a contaminated surface, and then touch their eyes, nose or mouth.
We are less certain on the fatality rate of Covid-19, but experts are working hard to collect data on the case fatality rate, which means the risk that someone who develops the disease will eventually die. Calculations from available data suggest this rate is around 2%, making it more deadly than seasonal flu (~0.1%), but far less deadly than some coronavirus diseases that affect humans, which include SARS (~11%) and MERS (~35%). This number will change over time, as we gain a better understanding of how many people have actually been infected with the virus.
There’s clear evidence that, much like seasonal flu, the risk of death increases depending on an individual’s age and whether they have underlying health conditions. The elderly and immunocompromised are the most vulnerable groups. Adults with underlying heart or respiratory conditions, including smokers and those with diabetes, also have a higher chance of developing fatal complications.
How do you test for Covid-19?
There are two types of test.
1. A test to show if someone currently has the coronavirus
This test indicates whether someone has the coronavirus and therefore their condition needs monitoring. Nose and throat swabs are taken from patients, and the test – called real-time reverse transcriptase PCR – looks for the genetic sequences specific to the virus.
Nearly all of the testing currently happening around the world is done this way. It is highly accurate, but each test has to go to a lab for analysis, so it can be time-consuming and needs specialist training.
Efforts have been made to scale-up the roll-out of these tests around the world. To support the effort in the UK, universities have been donating equipment and volunteering staff to work in dedicated diagnostic facilities. Wellcome has joined the UK government, academic bodies and partners in industry to support the UK’s diagnostic capacity.
A key research priority is to develop a rapid diagnostic test. This would enable faster detection of those infected and remove the need for specialised laboratories.
2. A test for antibodies against the virus, to show if someone has had it in the past
Research is continuing into the development of a test for antibodies against the virus, to indicate if someone has already had it, however mild their symptoms. Also known as serological testing, the aim of this is to determine if people are immune, and how long immunity lasts for.
It’s hoped these tests could be done at home. They could involve a finger prick blood test, giving a result in 15-30 minutes. However, despite a great deal of research currently happening, there is not yet a definitive test which is widely available.
Both tests have a crucial role to play in tackling Covid-19. Together, they provide vital information to help governments decide on implementing and relaxing physical distancing measures, and researchers to develop successful treatments and vaccines.
Pressing play on the video above will set a third-party cookie. Please read our cookie policy for more information.
What are the different tests for Covid-19?
There are two types. Test 1 is a test that shows if you're infected with the coronavirus. It involves analyzing nose and throat swabs to look for the genetic sequences specific to the virus. It's highly accurate, but each test has to be analyzed in a lab, so it can be time-consuming.
Test 2 is a test that shows if you've had the coronavirus. It involves analyzing blood samples for antibodies against the virus. The test shows if a person has been infected previously and might now have some immunity. Samples are usually tested in a lab, but it's hoped that finger prick blood tests could eventually give results at home.
From diagnosing infection to indicating potential immunity, each test has a crucial part to play in tackling Covid-19. And together, they could help governments decide on relaxing physical distancing measures and determine the success of vaccines and treatments.
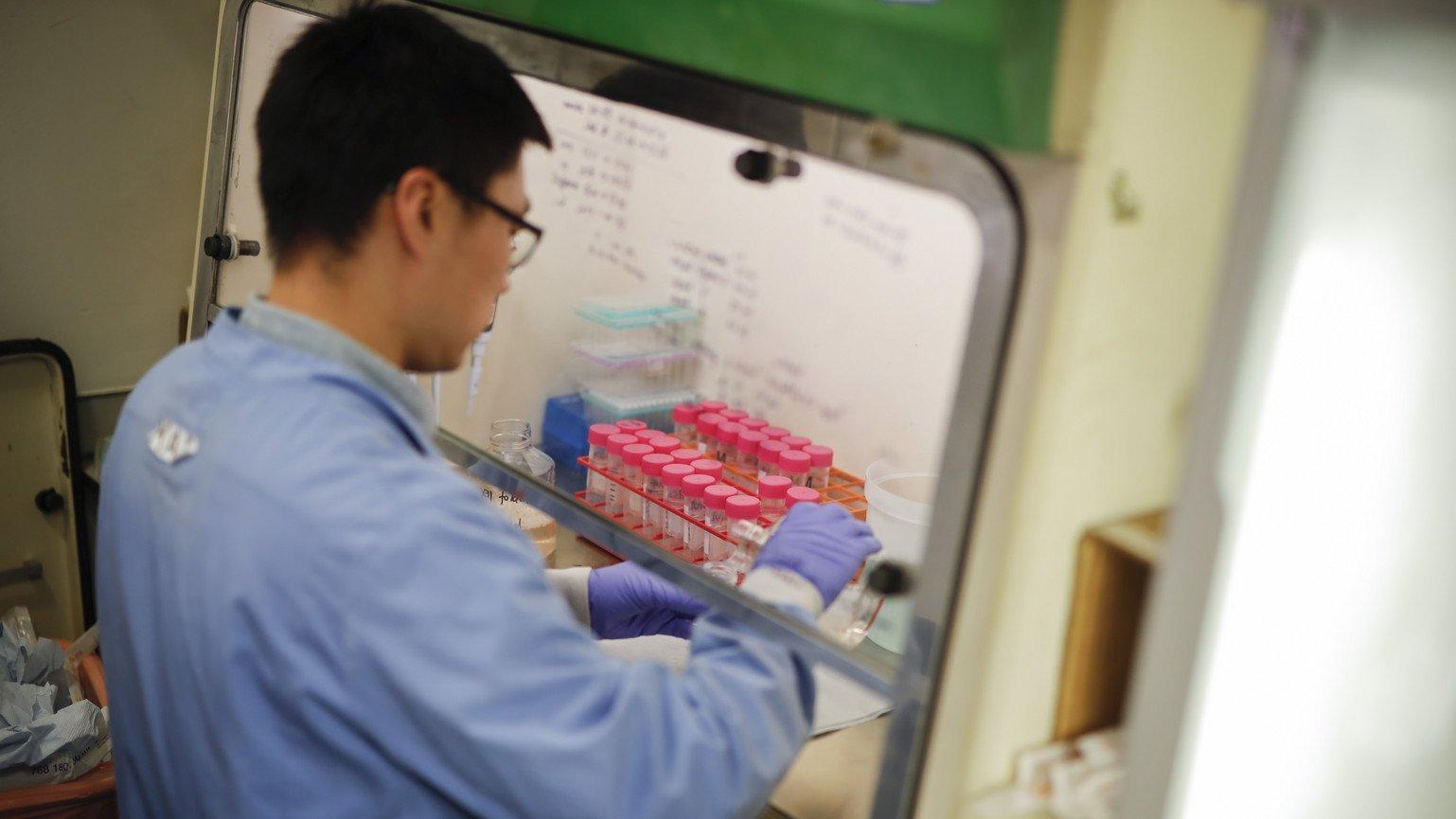
What research is being done on potential treatments?
There are currently no proven treatments for Covid-19. Companies and researchers around the world are working on potential treatment candidates, building on the research done in previous coronavirus outbreaks, such as SARS and MERS.
Clinical trials to investigate new treatments take time to set up. Launched by Wellcome, the Bill & Melinda Gates Foundation and the Mastercard Impact Fund, the Covid-19 Therapeutics Accelerator aims to speed up the research, development and manufacturing of potential treatments by evaluating new and repurposed drugs as soon as possible.
There has been considerable attention on the potential of hydroxychloroquine and chloroquine to prevent the spread of Covid-19. These drugs are used to treat malaria and lupus by targeting lung tissue, where the coronavirus is found, leading some researchers to think these treatments might be effective. The Therapeutics Accelerator has invested £7.5 million in a clinical trial to give a definitive answer.
To test other potential treatments, thousands of patients with Covid-19 in the UK have been enrolled on the Recovery trial. And the World Health Organization (WHO) has begun a multi-country Solidarity trial, including an investigation into Remdesivir – a drug that inhibits viral replication and was originally developed to target Ebola.
How close are we to a vaccine?
A successful vaccine will be critical to protect people against this and future outbreaks of Covid-19. It represents a crucial exit strategy to provide a path back to normal life, help protect health worldwide, and steer economies back on track.
Traditionally, vaccines take more than a decade to develop and license, and this process usually costs more than $500 million. When combined with the huge number of vaccine doses needed to stop Covid-19, the challenge faced is considerable.
Normally, a vaccine has to pass through multiple hurdles to be approved for use. However, in the global collaborative effort to find a Covid-19 vaccine, research is happening at an unprecedented pace with researchers, developers and funders working together to streamline the process. There are around 115 possible Covid-19 vaccine candidates in development. And some of the cutting-edge methods used during this outbreak could revolutionise vaccine development in future.
There’s no guarantee that the first vaccines in clinical trials will be the ones we need, and we will need a number of different vaccines. That’s why all these potential approaches must be fully supported and funded.
The Coalition for Epidemic Preparedness Innovations (CEPI), a global alliance Wellcome helped to found, is supporting the development of nine vaccines. Three of these vaccine candidates, developed by Moderna, Inovio and the University of Oxford, are already in phase 1 clinical trials – beginning just two months after the coronavirus was genetically sequenced.
Success is not guaranteed, but experts hope it will be possible to deliver a safe and effective vaccine in months. However, at least $2 billion of investment is still urgently needed to support vaccine development and another $1 billion for manufacture, so that we can make the billions of doses required to reach everyone who needs one across the world.
Pressing play on the video above will set a third-party cookie. Please read our cookie policy for more information.
We don't yet have a vaccine for Covid-19, but what we need to remember is that Covid-19 was only identified at the end of December 2019, so essentially it's less than five months old, and normally it takes more than ten years to develop a vaccine. It's likely that by the end of 2020, we'll have some clinical data on certain vaccine candidates from a safety perspective and also to tell us whether the vaccine shows signs of being protective. There are multiple challenges to developing an effective vaccine, which is why it normally takes more than 10 years to develop one.
Firstly, the speed at which we want a vaccine to be developed and available to everyone, and secondly, the scale, the number of doses that we want available. We want doses available for everyone in the world, ideally in the billions. There's no guarantee that we'll be able to develop an effective vaccine against Covid-19; this isn't a given. So, what a $2 billion funding gap means is that with the multiple candidates which are currently in early stage development, it might mean that some promising candidates may not be able to be taken forward. In essence, we have fewer shots on goal and fewer opportunities, fewer chances to develop an effective vaccine.
It could also take much longer, but I am optimistic. I do think that we are able to develop an effective and safe vaccine and that it will be available in the doses which we need. And when it is available, we need to ensure that it's accessible to everyone around the world because as long as one country still has Covid, we're all at risk.
How is research helping to measure and limit the spread and impact of Covid-19?
Researchers and healthcare workers are providing insights to inform global public health policies, such as encouraging good personal hygiene, enforcing physical distancing, and testing potential cases, therefore limiting the impact of Covid-19 on health services.
This research includes:
- Genome sequencing: the Wellcome Sanger Institute is working with partner organisations to sequence the Covid-19 genome for the first time. This will help us better understand how the virus is spreading on a national scale, and whether different strains are emerging, which will in turn help to improve patient care.
- Serology studies: a critical research question is how many people worldwide have had SARS-CoV-2, whether they are developing immunity to the virus, and for how long. Large-scale serology (or blood sample) surveys to identify antibodies the body makes after an infection are underway to help answer this. They will support research to find tools to prevent and treat the infection.
- Clinical data collection: the International Severe Acute Respiratory and emerging Infection Consortium (ISARIC) is collecting clinical data on Covid-19 from around the world, which is helping to give insights into patient characteristics, treatment success, and comparisons between countries.
- Mathematical modelling: modellers are mapping the latest reported disease characteristics, shared by governments and the WHO, to travel and behavioural patterns and estimating where disease is spreading and how quickly. When coupled with test results, this information can be used to accurately predict the outcome of different public health measures.
- Research to support low- and- middle income countries: in partnership with the Department for International Development (DFID), we’re supporting projects to help countries with weaker health systems and vulnerable populations prepare for the pandemic through research.
How can we make sure that everyone has equal access to vaccines, treatments and tests?
The Covid-19 virus has reached every corner of the world. As long as it is out of control somewhere, it is a threat to us all.
All research and development funders, manufacturers, developers and governments must engage with each other to make sure that new vaccines, diagnostics and treatments developed for Covid-19 are globally available, appropriate and affordable, regardless of where they have been developed or who has funded them. Otherwise Covid-19 will turn into a recurring global threat.
And it’s vital that everyone around the world has equal access to any scientific advances, and that research findings and data are shared rapidly and openly, helping researchers to develop effective vaccines, diagnostics and treatments more quickly.
How is research into Covid-19 being coordinated globally?
To chart the path that global research and development needs to take, the WHO, supported by a range of partners including Wellcome, have published a Research & Development Blueprint and a plan of immediate and longer-term priorities which has formed the basis of the WHO coronavirus roadmap.
The UK Collaborative on Development Research and the Global Research Collaboration for Infectious Disease Preparedness have also developed a tool that will help funders and researchers identify Covid-19 research and funding gaps.
However, at least $8 billion is needed to cover a funding shortfall for global Covid-19 research and development.
It will take a monumental global effort to tackle the virus. And we urgently need investment from governments, businesses and philanthropies – including many funders not usually involved in public health – fast, at scale, without any thought of a financial return.
Research remains the world’s best exit strategy from Covid-19 and this initial funding boost – a fraction of what governments have found to protect their economies – would provide the resources needed both to develop diagnostics, treatments and vaccines, and to scale-up production across the world.
Wellcome has launched COVID-Zero, an opportunity for businesses to donate to and advocate for this society-wide effort, playing a critical role in ending the pandemic.
Pressing play on the video above will set a third-party cookie. Please read our cookie policy for more information.
We must put research at the heart of any pandemic.
This is a global emergency. We need research at a global scale because research is the way out of this pandemic. It means we can get better at testing, find treatments that work, develop vaccines to protect us, and stop it happening again.
But time is precious. Governments can stop it, but we need them to invest. We need them to invest in global research, and we need them to invest now.
Research held immense power against Ebola. Together, we were able to develop vaccines, treatments, and testing faster than ever before — but only because we put research at the heart of the epidemic.
But to make all this happen, we need at least $8 billion urgently to fund global research for the current Covid-19 outbreak.
So let's come together, let's invest in research, let's outsmart this pandemic. Let's save lives.
How can research into this outbreak prevent future epidemics?
Putting research at the heart of the response is a double win – helping to fight outbreaks that are underway and protect us in future. This is something we’ve seen in response to Ebola which, thanks to the commitment to research during the last two outbreaks, is now a disease which can be diagnosed, prevented and cured.
Research is crucial to ending the Covid-19 pandemic. It is highly likely there will be future waves, so having the right treatments to save lives and one or more vaccines is absolutely critical.
And the research done now will help us to tackle future epidemics when – not if – they happen again. The lessons learned must be used to strengthen existing health systems and support low- and middle-income countries, where health systems and economies are often disproportionately devastated.
With continued investment, supported by political will, private-sector involvement and the help of the WHO and other multilateral bodies, we can prepare today to stop future outbreaks spiralling into health emergencies.
The WHO has already prioritised a number of other diseases that pose a risk to public health because of their epidemic potential, and the global health community is working hard to fill the knowledge gaps.


