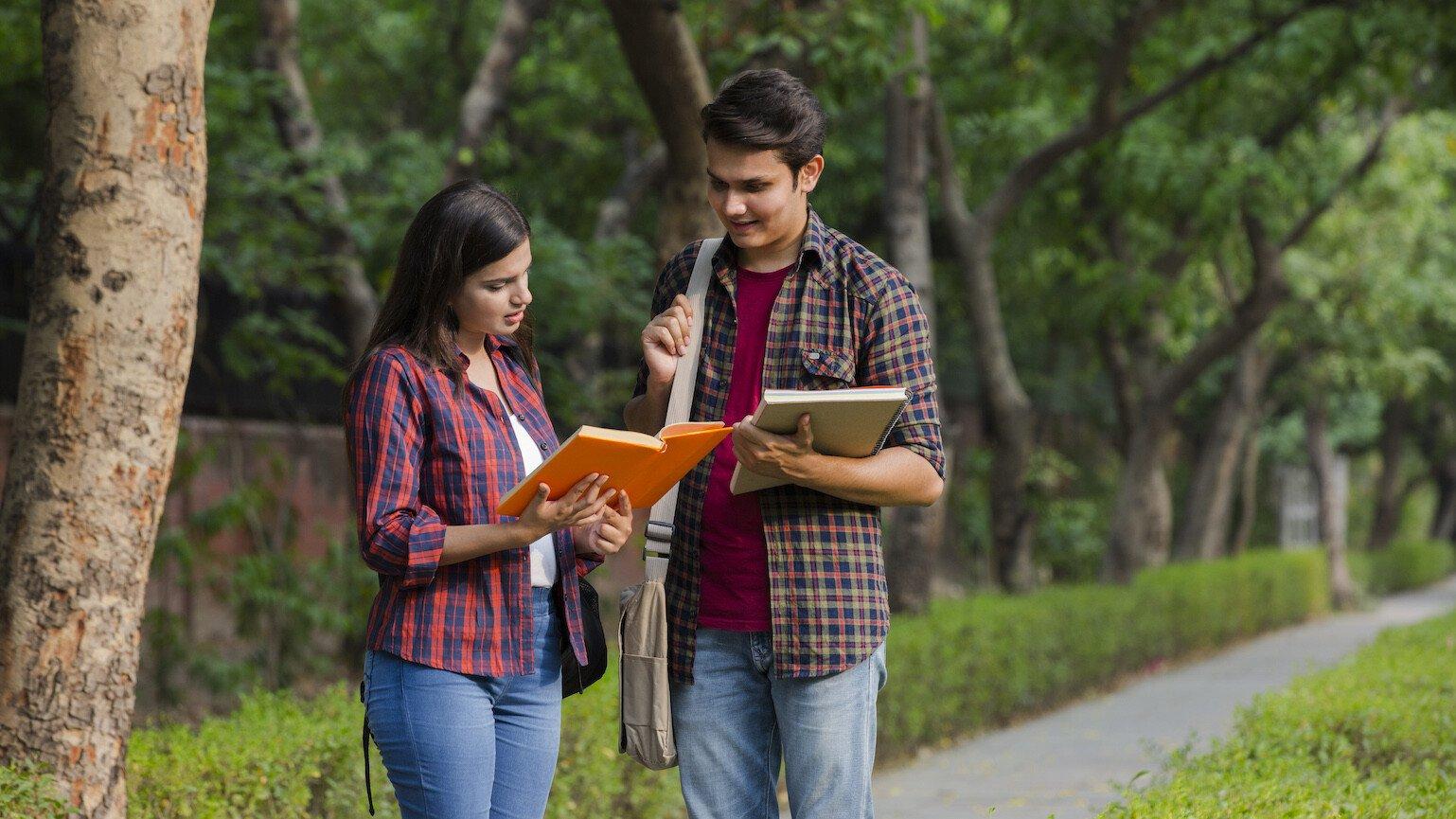
University students are at risk of depression – could peer-led interventions help, and if so, how?
7-minute read
Mental health problems like depression are common among university students. This research team will design, deliver and evaluate low-cost, peer-led interventions that could improve student mental health in India and beyond.